Linking Oral Health to Chronic Disease Prevention
Poor oral health—particularly periodontitis—is not just about cavities or bad breath. Growing research highlights Linking Oral Health to Chronic Disease Prevention, with implications for cardiovascular health, diabetes control, and more. A 2025 narrative review underscores how managing gum inflammation can significantly reduce the burden of systemic conditions .
1. The Oral-Systemic Connection
Periodontal disease is a chronic inflammatory condition of the gums and tooth-supporting structures. This inflammation doesn’t stay localized—it can trigger systemic cytokine release, elevating markers like CRP, IL‑6, and TNF found in heart disease and diabetes .
An umbrella review also confirms strong, bidirectional associations between oral diseases and at least 28 noncommunicable diseases including cardiovascular disease, diabetes, rheumatoid arthritis, obesity, inflammatory bowel disease, and certain cancers .
2. Key Chronic Diseases Affected
Cardiovascular Disease (CVD):
Oral bacteria and inflammation may enter the bloodstream, promoting atherosclerosis, high blood pressure, and higher risk of heart attacks and strokes .
Diabetes Mellitus:
Diabetes worsens gum disease, and untreated periodontitis impairs glycemic control. Conversely, periodontal treatment can help stabilize blood sugar levels .
Inflammatory Bowel Disease (IBD):
Emerging evidence suggests an oral-gut axis—oral pathogens migrating to the gut may exacerbate inflammatory gut conditions .
Rheumatoid Arthritis & Other Autoimmune Conditions:
Persistent oral inflammation may increase systemic inflammatory burden, contributing to autoimmune disease severity .
Cancer & Cognitive Health:
Poor oral hygiene has been linked to oral and head/neck cancers and potential risks for neurodegenerative conditions like Alzheimer’s via chronic inflammation pathways.
3. Mechanisms Behind the Link
Your mouth is not separate from the rest of your body—what happens there can affect your overall health. One of the biggest reasons is inflammation. When you have gum disease (like bleeding or swollen gums), your body is constantly fighting infection. This causes ongoing inflammation, which can spread through your blood and affect other parts of your body. This type of long-term inflammation has been linked to serious health problems like heart disease, diabetes, and even some types of cancer.
Another way your mouth can impact your health is through bacteria. The germs in your mouth—especially if you have poor oral hygiene—can get into your blood when your gums bleed. Once these bacteria travel through the body, they may reach your heart or other organs and cause more problems.
There’s also a two-way connection between Linking Oral Health to Chronic Disease Prevention. For example, if someone has diabetes, it becomes harder for their body to fight gum infections. At the same time, gum disease can make it more difficult to control blood sugar. So, one problem makes the other worse.
In short, keeping your mouth clean and your gums healthy doesn’t just give you a nice smile—it helps protect your heart, blood sugar, and your entire body from serious health issues.
4. Insights from D’Aiuto et al. (2025)
Treating periodontitis offers more than just oral health benefits—it may help reduce the burden of chronic diseases, improve patient outcomes, and lower overall healthcare costs. By linking oral health to chronic disease, this review highlights the need for integrated screening protocols in medical settings, particularly for individuals with diabetes or cardiovascular conditions. It urges dentists and physicians to establish strong referral pathways, promoting coordinated, bidirectional care for better long-term health.
5. Practical Tips to Optimize Oral & Systemic Health
1. Brush twice a day and floss daily, replacing your toothbrush every 3–4 months .
2. Regular dental check-ups—ideally every 6 months—to detect early signs of gum disease.
3. Screen for chronic diseases in dental settings (e.g., hypertension, high glucose) and refer as needed .
4. Manage shared risk factors: stop smoking, control sugar intake, maintain healthy weight, and manage diabetes.5. Adopt nutritional support, including vitamin C, D, and K for periodontal healing and bone health .
6. Downstream Benefits of Oral-Systemic Integration
By integrating oral care into chronic disease prevention strategies, health systems can:
- Detect systemic illness early via oral-screening touchpoints.
- Improve chronic disease management through reduced inflammation and better patient engagement.
- Lower healthcare costs by preventing complications and hospitalizations .
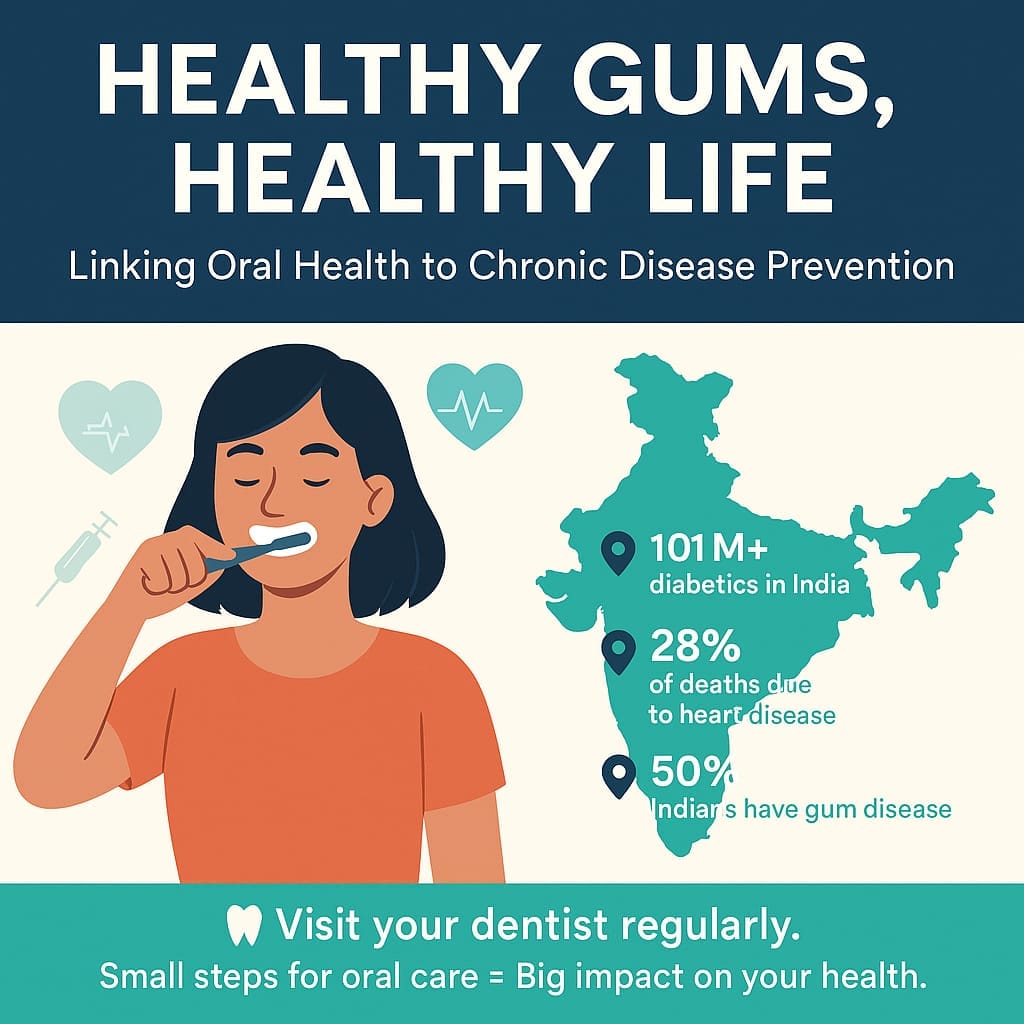
India-Specific Insights
1. High Prevalence of Periodontal Disease in India:
Over 50% of Indian adults suffer from some form of gum disease, often undiagnosed due to lack of awareness and regular dental checkups. (NIH India Data 2024)
2. Diabetes & Oral Health in India:
India is the diabetes capital of the world with 101 million diabetics (as per ICMR 2023). Periodontitis worsens glycemic control and is common in diabetics.
3. Cardiovascular Disease is the No. 1 Killer in India:
According to the Global Burden of Disease Study, CVD accounts for 28% of all deaths in India—periodontal bacteria have been implicated in atherosclerosis.
4. Low Access to Oral Care in Rural Areas:
About 72% of India’s population lives in rural areas, but only 20% of dental professionals serve these regions. This limits access to early periodontal treatment and chronic disease screening.
5. Tobacco Use & Oral Cancer Link:
India has the highest number of oral cancer cases globally, largely due to smokeless tobacco and poor oral hygiene, compounding chronic disease risks.
Conclusion
Oral health is far more than cosmetic—it’s a gateway to chronic disease prevention and better overall health. D’Aiuto et al. (2025) and related research collectively show that managing periodontitis and promoting routine oral care can reduce systemic inflammation and lower risks for diseases such as heart disease, diabetes, IBD, and more.
Medical and dental providers must work collaboratively through shared screening protocols and referrals to enable holistic patient care. And individuals can take charge through consistent oral hygiene, nutrition, and regular check-ups. Start with your mouth—protecting it helps protect your life.

Leave a Reply